Existing turbulent healthcare industry scenario :
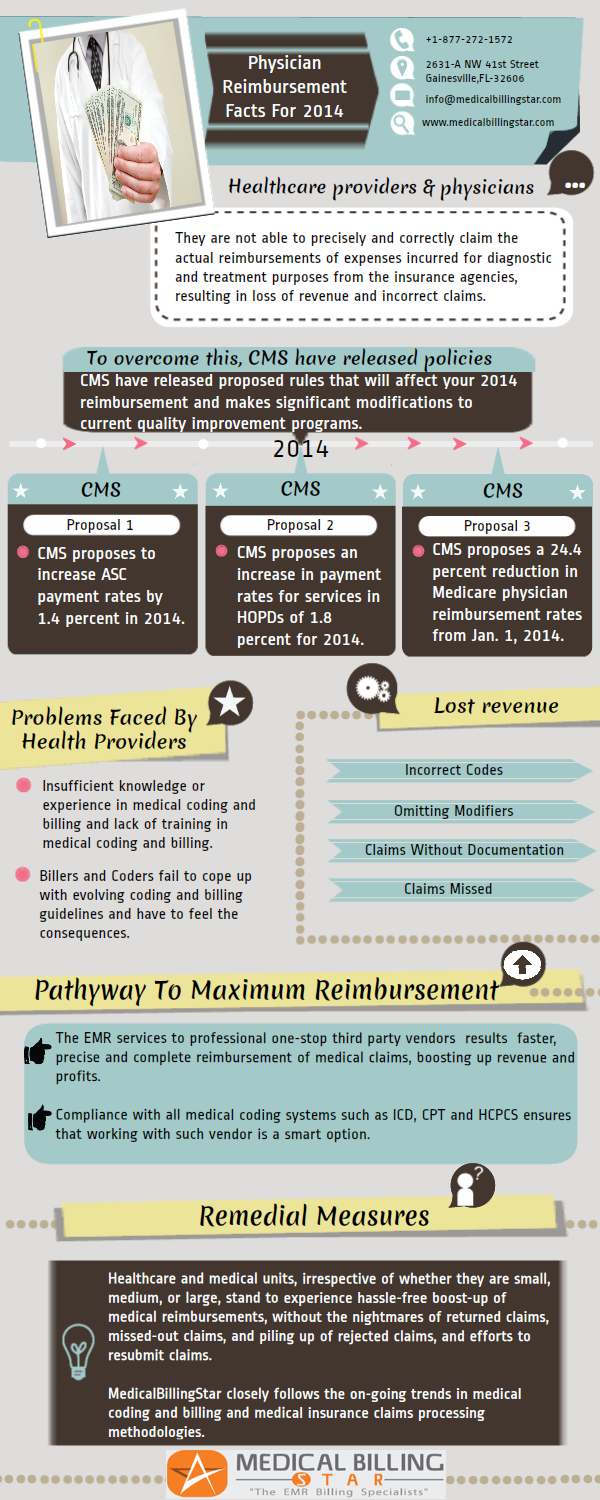
In the current turbulent economy-ridden environment healthcare providers and physicians are not able to precisely and correctly claim the actual reimbursements of expenses incurred for diagnostic and treatment purposes from the insurance agencies, resulting in loss of revenue, profitability, incorrect claims, delayed claims, missing out on claims, the main reason being that they are not fully equipped to provide precise diagnostic and treatment documentation, backed by capturing the correct medical codes for medical billing. The physicians do not have the time to oversee capturing the correct medical codes and medical billing procedures as they have to focus on their core competency of diagnosis and treatment as first priority.
Vital issues compounding the problems :
Healthcare professionals are constantly under pressure due to increased patient/financial constraints and regulatory pressures, forecasting a doomsday for medical services. This situation is worsened further due to federal regulations that advocate improved, affordable healthcare services without comprising on quality issues even under the present economic scenario where the inputs for provision of healthcare services are experiencing spirally increased costs. To further complicate the issue, in-house administrative personal are not inadequately trained, inexperienced and lack the requisite expertise in medical coding and billing, as well as thorough and accurate clinical documentation.
The physicians would like to spend most of their time and efforts by focusing on core issues of diagnosis and treatment, rather than diverting their resources and energies over the nuances of managing and monitoring their to maximize revenue. Rather than have in-house medical coding and billing services, it pays to opt for outsourcing or right sourcing the billing services to established and experienced vendors. There is a dire need for in-house analysis of existing problems, solutions, future trends, and remedial measures.
The situation will further worsen in the near future since presently health care reforms are under way with focus on affordable health coverage and quality.
Medical Reimbursement Problems faced by Health Providers :
- Insufficient knowledge or experience in medical coding and billing
- Lack of training in medical coding and billing
- Physicians using In-house medical coders and billers have to feel the consequences by struggling with inexperienced coders straight out of college
- These billers and coders fail to cope up with evolving coding and billing guidelines, for medical procedures, and stay abreast with the latest procedures
- Nightmares of lost revenue and unpaid bills
Lost revenue opportunities :
- Physicians tend to miss opportunities to maximize medical reimbursements from the insurance companies.Lost revenue due to various factors includes:
- Undercoding level of treatment,
- Omitting modifiers,
- Submission of medical reimbursement claims without the requisite documentation required to support the reimbursements.
- Wastage of resources in determining and tracking reasons for claims rejected, besides finding out claims missed or under claimed.
The pathway to maximum reimbursement :
- Out sourcing or better known as “Right sourcing” the medical billing and coding, clinical documentation, claims processing, EMR services to professional one-stop third party vendors results faster, precise and complete reimbursement of medical claims, boosting up revenue and profits.
- Besides assigning the right codes for medical services the outsourcing vendor provides specialty specific coding services using experienced and AAPC credentialed coders on board.
- The vendor is conversant with the significance of coding for the technical and professional components of a medical service, place of service codes, e/m codes, revenue codes, and when claims need to be bundled or unbundled.Compliance with all medical coding systems such as ICD, CPT and HCPCS ensures that working with such vendor is a smart option.
Remedial Measures :
- Wise,prudent, and strategic to partner established third party vendors such as MedicalBillingStar who have long-standing expertise, experience in dealing with state-of-the-art coding and billing services to a wide range of categories in the US medicare industries.
- Healthcare and medical units, irrespective of whether they are small, medium, or large, stand to experience hassle-free boost-up of medical reimbursements, without the nightmares of returned claims, missed-out claims, and piling up of rejected claims, and efforts to resubmit claims.
- MedicalBillingStar closely follows the on-going trends in medical coding and billing and medical insurance claims processing methodologies.