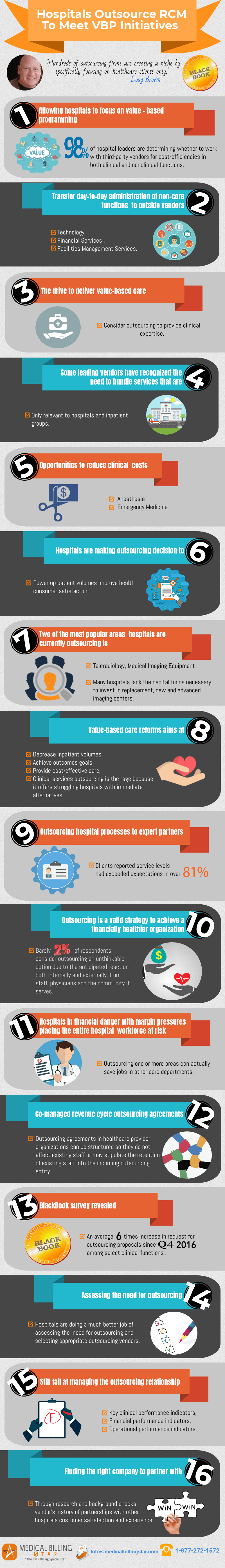
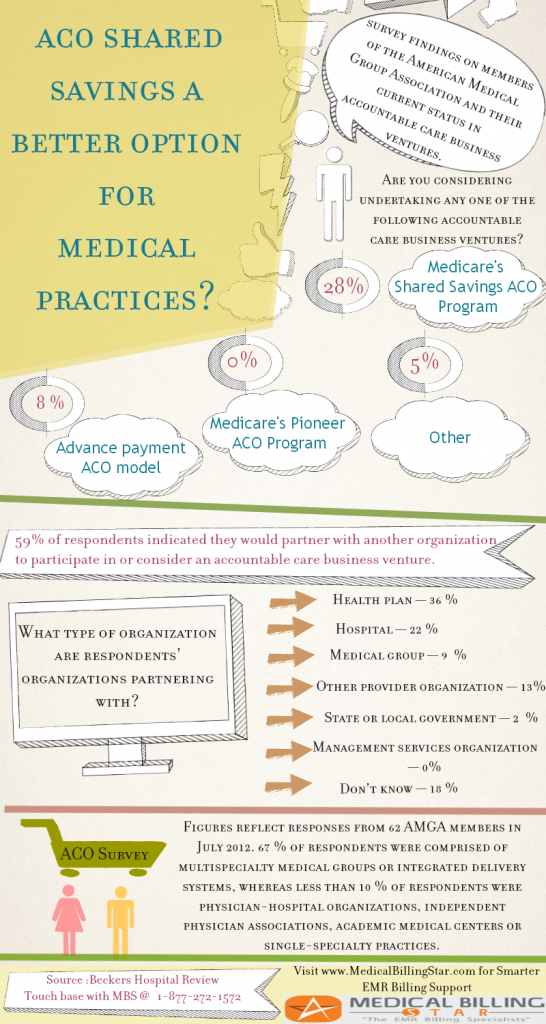
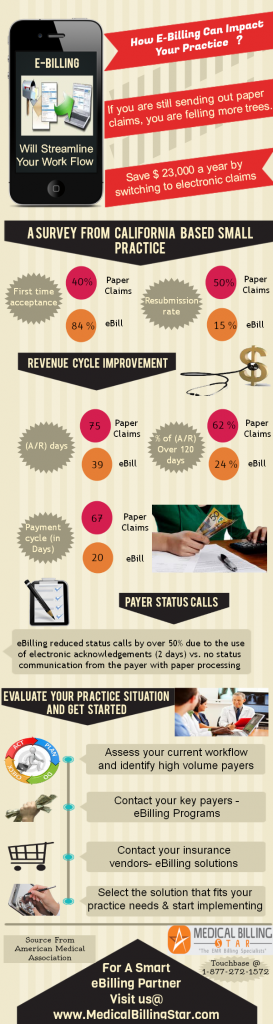
The value-based care payment reform is a huge game changer. It has brought about vast changes in the way hospitals manage their billing and revenue cycle operations. This infographic tracks the changes brought on by the payment model that has drastically altered the way healthcare organizations handle their RCM process.
Conclusion: All these statistics and facts point towards one trend- the emerging and burgeoning need for RCM providers to bail healthcare organizations out of this tricky phase. Please share out this infographic if you find it useful.