Well, it is not a war in the strictest sense of the term, but it does denote the recent developments in the ACO or Accountable Care Organization scene where many Pioneer ACOs have been opting out of the program due to difficulties in meeting the targets and the high risks involved. About 25% of the Pioneer registered Accountable Care Organizations are in the process of exiting the program and joining the lower-risk option, the Shared Savings Program. CMS had this to say about the fallout :
“We’re encouraged that these organizations want to continue in programs that promote better care at lower costs, we fully anticipated that as these programs get up and running, some organizations would shift between models.”
Health Reforms & ACOs
For those of you, who have been too busy to register what an ACO exactly is, it is a category of CMS program, which is part of the government health reform, which includes others like Patient Centered Medical Home, Medical Neighborhood, Health Home, etc. The reforms themselves consist of three main components, which is a superset of any practice models. They are :
a. Care Delivery Reforms.
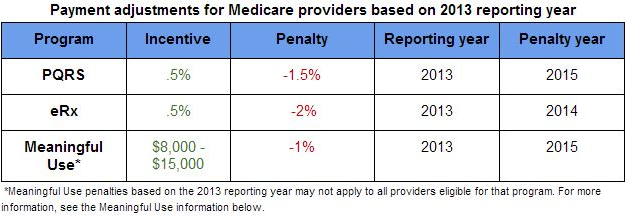
b. Payment Reforms.
c. Health and Healthcare Community Reform.
ACO is a model which is, to quote a popular definition, “an organization, virtual or real that agrees to take on the responsibility for providing care for a particular population while achieving specified quality objectives and constraining costs.”
As the above definition clearly points out, an ACO platform is expected to stimulate more integrated care for the patients, which would ultimately result in quality improvements and healthcare cost reduction. Also, in these programs the ACO gets a share in the costs ultimately saved.
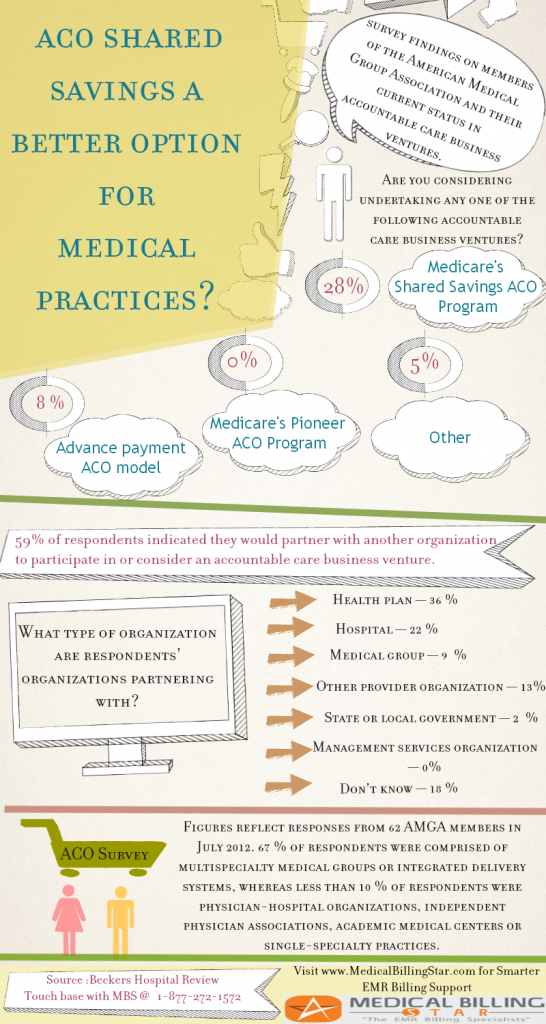
Pioneer vs Shared Savings Programs
SSP and Pioneer were two landmark ACO programs created by CMS. The latter has a slightly complex format, which takes into consideration organizations that already have some experience in providing coordinated care.
The Main Differences between the two are:
1. SSP has two payments tracks and it is upto to the ACO to choose either the non-risk sharing one (which has less cost savings share) and the risk-sharing track (which has higher cost savings share but at the same time there are possibilities of losses upto even 60%).
2. The Pioneer utilizes a trending methodology that, all other things being equal, produces a slightly higher benchmark than the SSP for high-cost areas.
3. The SSP will need to cater to at least 5,000 Medicare fee-for-service beneficiaries, whereas the Pioneer needs to service 15,000.
4. The Pioneer program importantly includes a clause that 50% of Pioneer ACOs revenues should come from participating in “risk” contracts with other non-CMS (private) payers.
The Significance of events such as the above
Republicans have been ardently opposing the health reforms (which is really an attempt for universal healthcare). The recent refusal by the National Football League to team up with the government to promote ObamaCare has been touted as some sort of vindication for their stance. Also, the refusal of some states to adopt the Medicaid expansion plan and the setting up of online HIE, to realize the goal of “healthcare for all” , is seen as further supporting evidence. And the above developments in the Pioneer ACO scene is construed by some health reform detractors as the “straw that will break the ACO camel’s back”.
MedicalBillingStar : A Voice of Sanity
With a decade of hands-on experience in servicing over 500 clients when it comes to the RCM Cycle, MedicalBillingStar always endeavors to float above the cacophony of healthcare gossips and half-truths, to provide their medical billing and coding clients with information that is relevant, besides of course catering to their entire RCM workflow. We are aware of the impact that ACO’s will have on payment models, the changes from which ultimately have to be incorporated into the RCM process. Thus, we keep abreast of the latest happenings in the payment model scene. Meanwhile you may call MedicalBillingStar at 877-272-1572 or visit our website at www.medicalbillingstar.com if you any questions about any of the above or the Medical Billing/Coding processes in general.