The E-gadget Backdrop
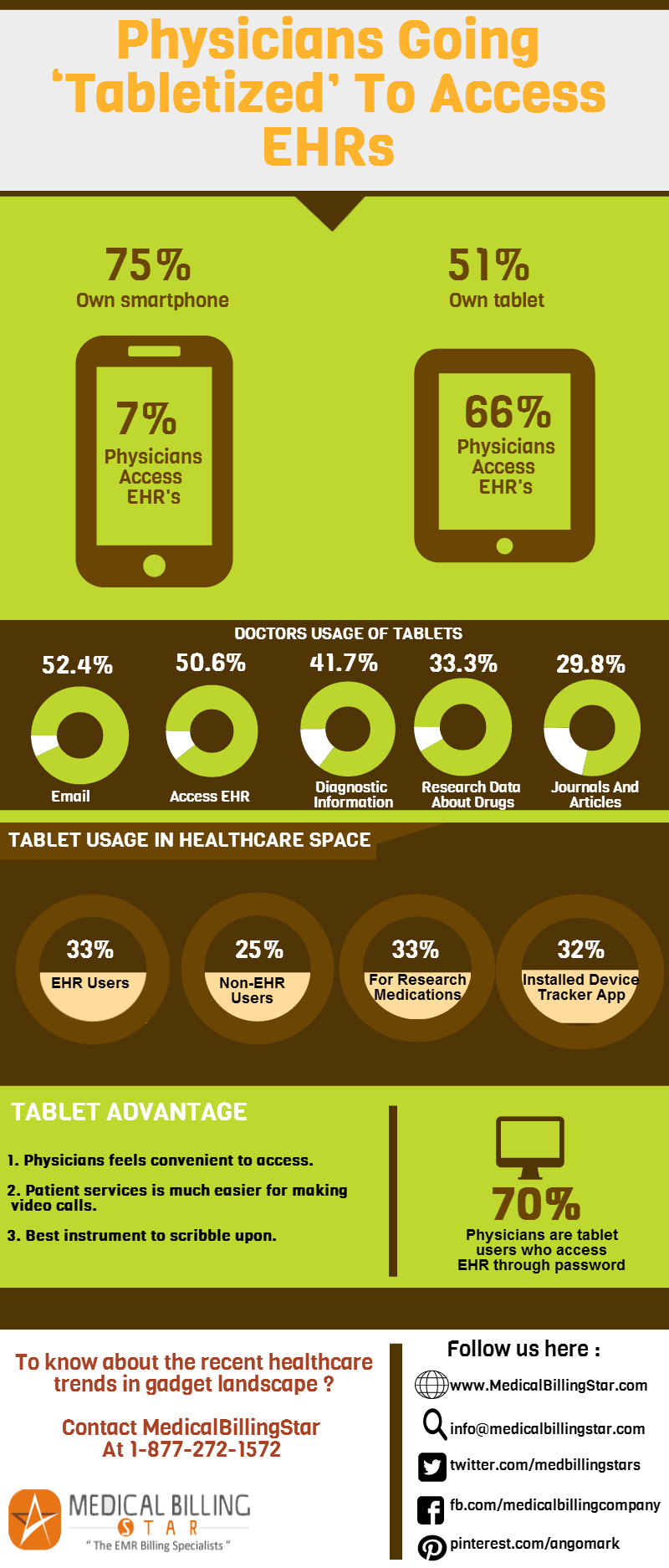
The mobile gadget revolution in the healthcare arena is at the cusp of ‘tabletization’, according to a string of new reports. Clinicians are increasingly using their mobile devices, especially tablets at practices for the rapid, secure and amicable electronic health records’ (EHRs’) usage, storage and exchange.
Insights into the Penchant for Tablets
It’s a trendy ‘spectator sport’ among new practices and the mobile purveyors to fathom why physicians are utilizing their tablets. Two recent reports, “Mobile Usage in the Medical Space 2013″ and “Tablet Usage by Physicians 2013″ from American EHR Partners based on the survey of about 1,400 physicians, underscored that tablets are more useful than smartphones for doctors using EHRs.
The doctors use their tablets in the clinical settings for performing the following activities :
- 1. Sending and receiving e-mails (52.4 percent);
- 2. Accessing electronic health records (EHRs) (50.6 percent);
- 3. Retrieving diagnostic information (41.7 percent);
- 4. Research data about drugs (33.3 percent);
- 5. Keeping abreast with medical field through journals and articles (29.8 percent).
Snapshots on Tablet Usage in Healthcare Space
- 1. Physicians use Epocrates®, Medscape®, Up To Date®, MedCalc®, and Skyscape® as the top five tablet apps in their medical practices.
- 2. Smaller enterprises, with three doctors or less, are expected to carry out an extensive range of bustles on their tablet, such as banking, patients’ correspondence, or taking snaps for medical research, etc.
- 3. One-third of EHR users and one-quarter of non-EHR users prefer a tablet gadget in their clinical practice.
- 4. The users of EHR are hanging about 25 hours per week on their tablet device, with a better portion of time used up on business (59 percent) than for personal points (41%).
- 5. With an increased clinical and healthcare research funding, the research about medications is escalating. About 33 percent of EHR users employ a tablet to research medications every day.
- 6. About 70 percent of the physicians are tablet users who access EHR through password.
- 7. More than 32 percent have installed device tracker apps on their tablets, so as to remotely clear all data on their tablet – if misplaced or stolen.
Tablet- Benefits Overwhelm !
- A. Though smartphones and tablets are competitively used by physicians, most physicians are feeling convenient with the EHR access on a portable, wider screen as in tablets.
- B. Making video calls to interact with patients for research, feedback and patient services is much easier and pleasing with this device.
- C. During business meetings and even during special patient encounters, this is a great instrument to scribble upon.
Contact MedicalBillingStar to know about the recent healthcare trends in gadget landscape !