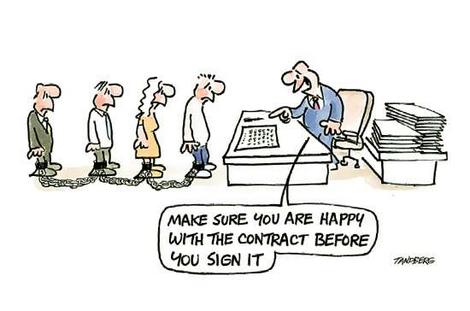
 Contract negotiation: Start on the right foot!
Contract negotiation: Start on the right foot!
You file claims regularly and follow up on them diligently. But why are the collection figures so dismal? It becomes a challenge to make ends meet and make a decent profit. Don’t look at your collections report. The cracks lie elsewhere and it’s never too late to make course corrections.
Payer contracts are usually overlooked and this oversight can cost your medical practice thousands of dollars a month. The major reason why negotiating payer contracts are usually never paid the attention it deserves, is because of a convoluted process that can take months on end to reach fruition.
At a busy medical practice nobody has the time to pore over contractual agreements, deduce fine-print and follow up with insurers. But medical billers should pay attention to payer contracts so revenue doesn’t slip through the cracks.
Are you making these 5 contract negotiation mistakes?!
#1. Not getting out unproductive contracts can put practices at a serious disadvantage. Billers should educate medical practices about how some “evergreen” contracts that get automatically renewed are detrimental to the organization and the procedures to break away from them.
#2. Most medical billing teams or firms do not run comparison reports with other medical practices. Not doing so can result in a stagnant revenue cycle and archaic payment structures. It is essential to keep an ear to the ground and change contracts according to recent payment regulations.
#3. Most billers do not perform consistent revenue analysis. Reimbursement analysis has to be performed regularly to check if the current prices are not outdated or under-priced.
#4. Payment models will have to be chosen according to the workflow, patient population and compliance requirements of the clinic. Contacting insurers and performing contract negotiations beforehand can actually be counter-productive.
#5. Not following up regularly with insurers regarding contractual changes is another major flaw. Medical billing teams or companies should follow up regularly with insurers to wrangle out the best possible contract.
Quick tips from the experts…
Foster relationships Like physicians, health insurers are under pressure to control costs and improve quality of care, and you can help them achieve those objectives.Discuss about areas of concern and how you can join hands to contain costs and improve quality of care
Stand out from the crowd The geographical location, size and specialty of a medical practice can affect the value an insurer places on your business. Look for what sets your medical practice apart and use it as your USP to negotiate better payments.
Read the fine print Make sure there is an annual renewal option . Also, pay attention, to notices of changes from your insurer. Every communication from the insurer should be scrutinized as it can contain important reimbursement information.
Beware of silent PPOs A silent preferred provider organization (PPO) can access discounted rates for services without your authorization, preventing you from billing patients for amounts above the contracted fee. So beware of them!
Source: http://www.physicianspractice.com/revenue-cycle-management/payer-negotiation-little-preparation-goes-long-way
