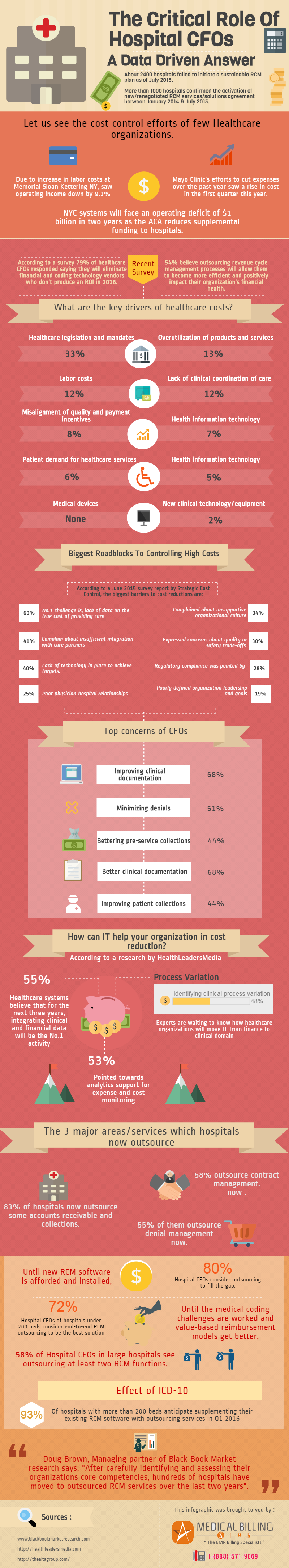
We know the evolving role of CFOs in the healthcare industry. There are situations which have forced the executives to make such decisions like changing the vendor, attritions and outsourcing one or more of their processes. There could be ample reasons like transition to value-based model, slow payer procedures, low Medicare and/or commercial payer reimbursements, ICD-10 etc.
Let me break this down into a data driven answer but before I want to share with you what medium and large healthcare organizations believe:
What do CFOs of medium healthcare organizations believe?
They make decisions as to clinical efficacy first and then cost management.
If a service is too costly to keep, there is consideration to drop the service as it deters from other services which are accretive to a positive margin.
What do CFOs of large healthcare organizations believe?
They focus on key opportunities for improvement
They put sufficient resources behind efforts to implement and hardwire improvement.
They don’t try to do everything at once.
Here are some facts and surveys which highlight the financial challenges of our healthcare industry leaders:
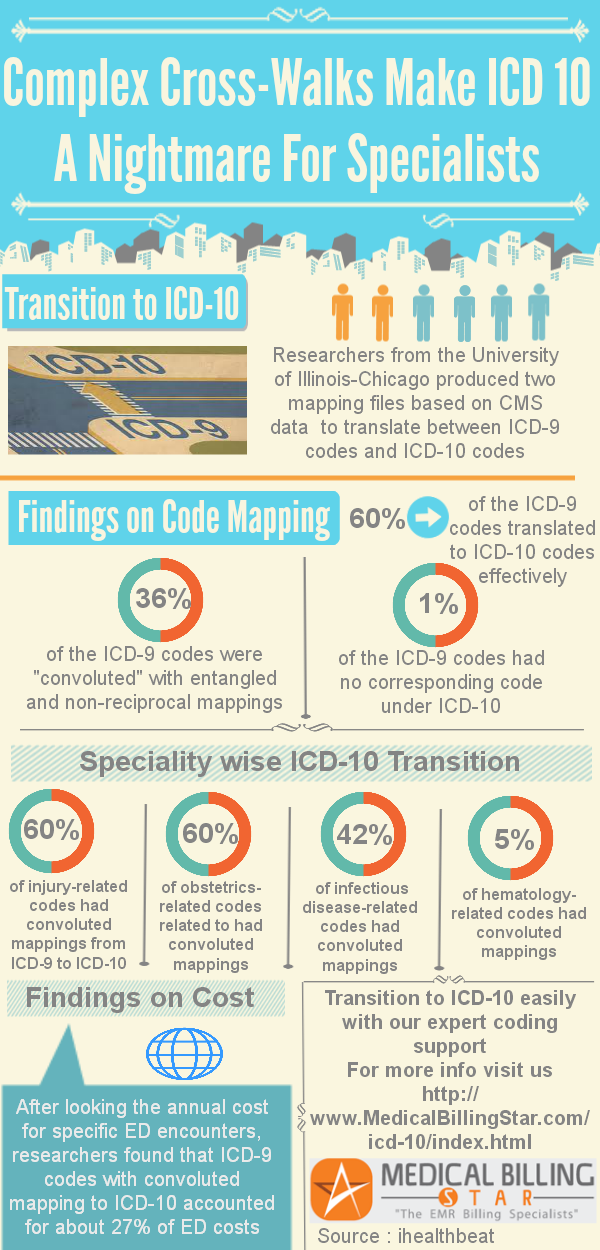
Click on the image below to enlarge: