EMR, a Marriage that has to succeed :
Healthcare providers in the US have opted for EMR as mandated by the federal government, for superior patient care and efficiency,with reduction in costs and enhancement of patient experience. However, the biggest hurdle, namely getting it to work efficiently, is not yet crossed.
Thorny path where benefits galore :
Implementation of an EMR system involves treading on a thorny transition path from paper-based to computer-based on-line live medical practice. However, once successfully implemented, improved efficiency, speed and accuracy of performing clinical tasks render the EMR systems an invaluable investment. It also promises to reduce clinician workload and medical errors.
The EMR Carrot :
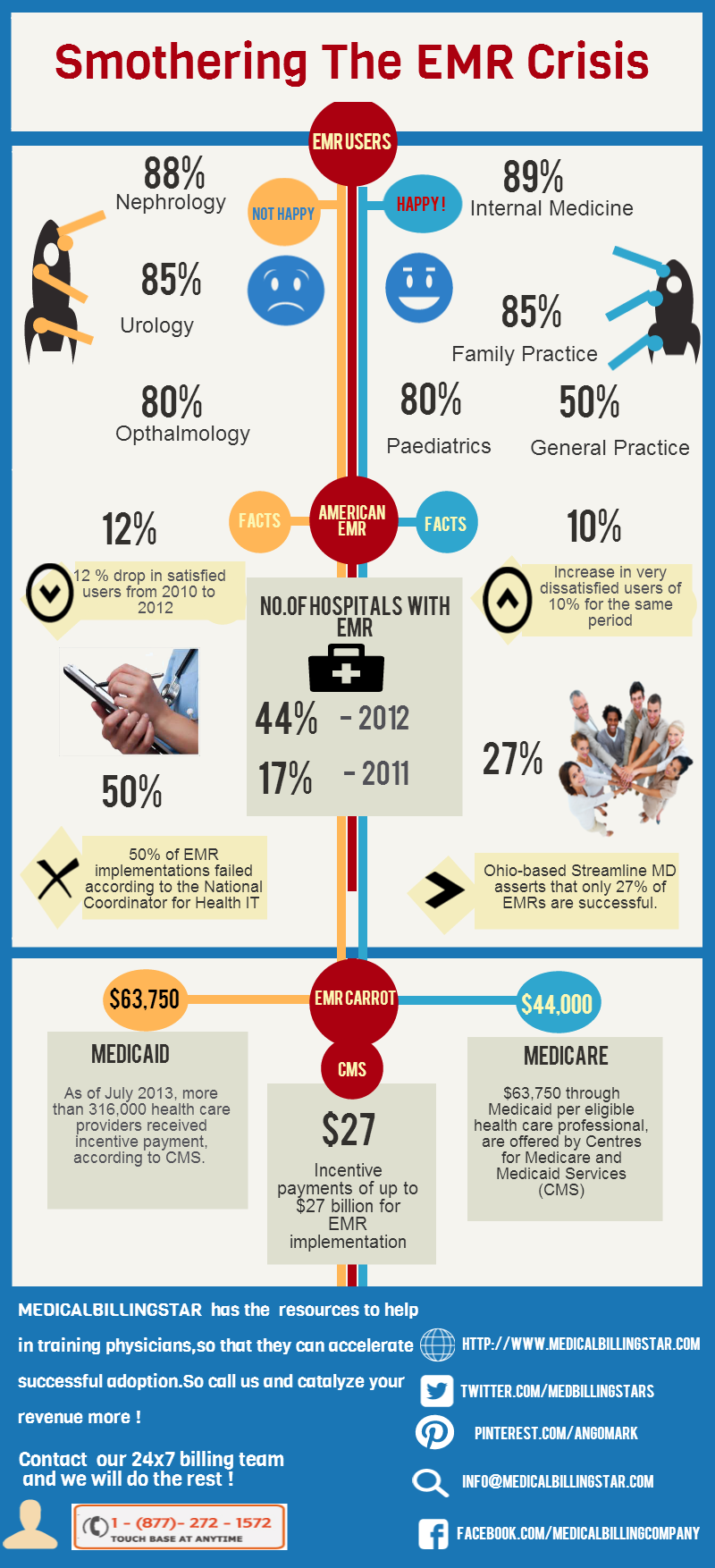
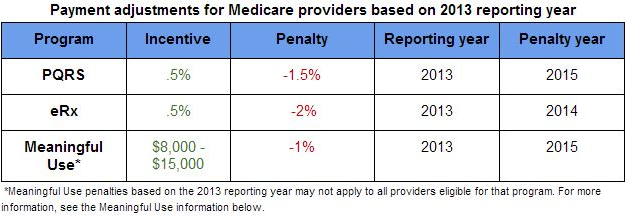
Incentive payments of up to $27 billion for EMR implementation, or as much as $44,000 (through Medicare) or $63,750 (through Medicaid) per eligible health care professional, are offered by Centres for Medicare and Medicaid Services (CMS). As of July 2013, more than 316,000 health care providers received incentive payment, according to CMS. According to the Robert Wood Johnson Foundation, the number of hospitals with EMR increased to 44 % in 2012, up by 17 % from 2011.
On the flip side,survey results depicta gloomy picture with yet to be realised EMR promises.
- 1. Based upon American EMR data collected from 2010 to 2012, user satisfaction levels with EMRs are dropping. These findings were presented at Healthcare Information and Management Systems Society (HIMSS) conference on March 5, 2013.
- 2. Overall EMR user satisfaction surveys revealed a 12% drop in satisfied users from 2010 to 2012 and a corresponding increase in very dissatisfied users of 10% for the same period.
- 3. Dissatisfaction with EMR implementation is increasing regardless of practice type or EMR system, asserts Michael Barr, MD, ofAmerican College of Physicians’ (ACP’s) .
- 4. 50% of EMR implementations failed according to the National Coordinator for Health IT
- 5. Ohio-based StreamlineMDasserts that only 27% of EMRs are successful.
- 6. Yes and No! A recent survey of 17,000 EMR users revealed that nephrology (88%), urology (85%) and ophthalmology (80%) practices expressed the highest rates of discontent with their EMRs, while internal medicine (89%), family practice (85%), general practice (82%) and paediatrics (80%) specialists experienced highest rates of satisfaction with their EMRs.
Reasons for the impasse: Lack of effective end user physician training in EMR is the bane across the US healthcare industry. Importance of training has been overlooked and under-estimated by physicians.Richard Stokes, director of sales for Network 1 Consulting, warns that continued inadequate training of physicians will slow down the EMR system implementation.
Way out of the doldrums: Need of the hour is effective EMR training that involves 8 important issues :
- 1. Tailoring the EMR training sessions specific to the hospital/clinic.
- 2. Using experienced and certified EMR trainers
- 3. One-on-one training: Every physician has a different learning curve. Hence, having one-on-one training is a must. For smaller practices that may not have advanced IT background, physicians should be made to initially work side-by-side with experienced trainers.
- 4. EMR training for everyday workflow: Training needs to bescheduled around normal physician practice workflow. The physicians should be made to use EMR consistently in the manner they’ll need towork after going-live.
- 5. Basic skills and practice procedures: Many physicians are not even familiar with intricacies of computer usage. They have to be familiarised with basic computer skills.
- 6. Train, retrain and retrain: Training never ends and is a true ally.Training patiently, retraining, and on-going training hold the key for success, adds Susan Miller, administrator at Family Practice Associates of Kentucky. Leann DiDomenico, administrative director of Performance Paediatrics, uses EMR training videos and makes the physicians repeatedly carry out their tasks on the EMR, until they are confident of performing on their own.
- 7. Avoiding rushed training sessions.
- 8. Continuous evaluation of on-going training.
Helping hand from MedicalBillingStar :
Hospitals and clinics in the US can bank on MedicalBillingStar as their EHR trusted partner to help train physicians in nuances of EMR implementation and functioning.Tailor-made EMR training modules are available to cater to the specifics of any clinic/hospital. Training options include formal training during office hours or in special sessions outside of normal business hours, offsite training, and online training.MedicalBillingStar has the resources to help in training doctors, so that they can catalyse successful EMR adoption.