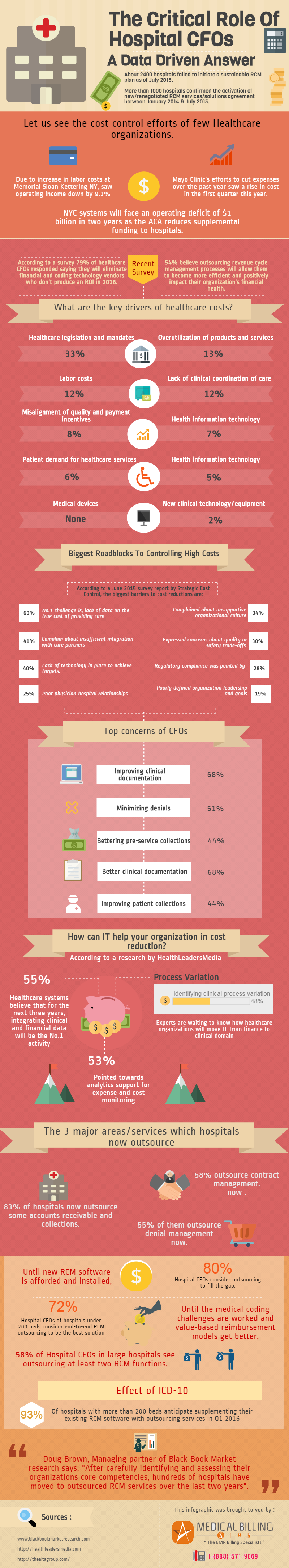
It is possible, depending on the practice size, you could be missing out on up to $100,000.00 dollars each month with little effort. Is this startling news to you? Have you done an analysis of what you should be collecting for co-pays? Have you compared this to the actual collections?
Co-pays
Co-pays are an integral part of the managed care program. You get a capitation check each month for the members you have in your practice. You are then expected to collect that co-pay for each member as they use your services.
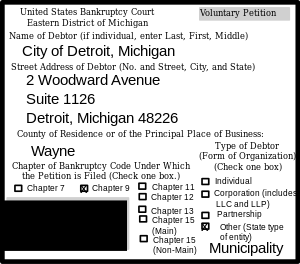
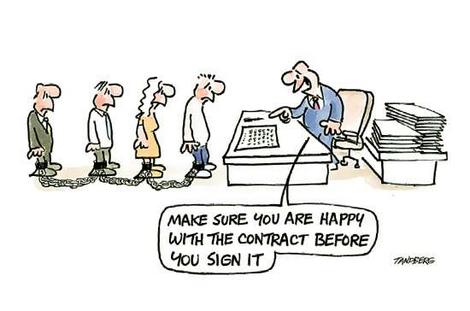
YES, I said “EXPECTED.” These co-pays are contractual obligations made by the patient when they signed up for their care. The managed care program is expecting you to be collecting this fee every time they are seen for a covered service. They base their fee reimbursement and your capitated check, in part, on those monies.
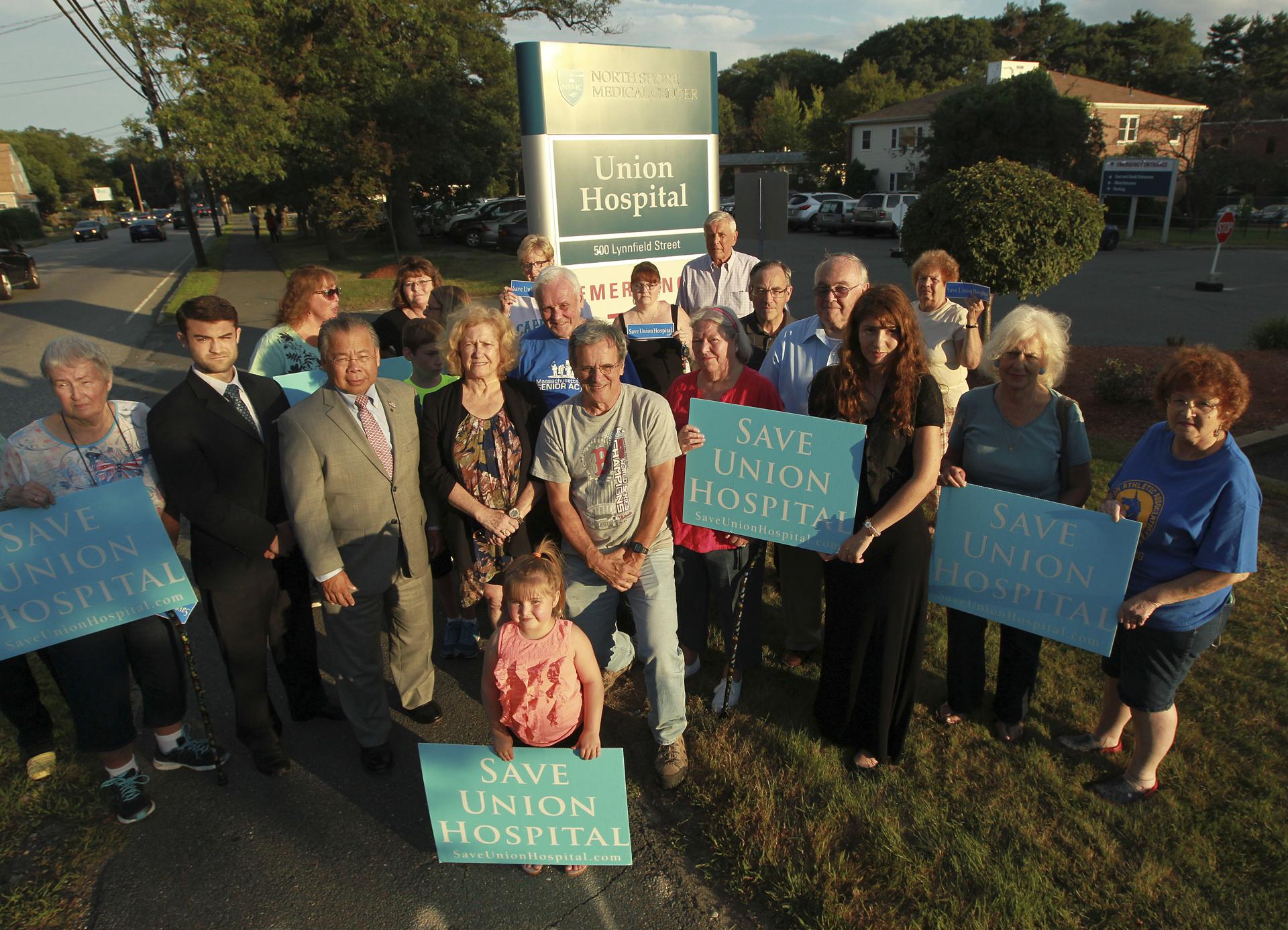
In many practices I have analysed, the front desk does not even broach this particular subject. Why? Usually, because there has been no expectation of this collection explained to them. This is a subject that must be explained and taught upon hiring and periodically reviewed both through observation and formal educational activities later in employment.
Educating patients is mandatory
The specific amount of patient education that must be built into this. Many patients do not know or understand what a co-pay is. Gentle explanations with reference to their insurance cards for guidance can usually clear this up. Explaining the importance of payment AT THE TIME OF SERVICE is the one concept that MUST be emphasised. This is many times exactly how the contract is written.
Think about this fact: It cost you approximately $8.45 to send and collect on monies owed. The more notices, the higher this figure goes. When co-pays are $5 or $10 you are losing a lot of money. When co-pays are higher, there is still a financial loss that could have easily been avoided.
This article will help you achieve your financial goals by pointing out the tried and tested methods that successful group practices follow.
Stressing contract law is not the way to go, but mixing this information in with other things the patient can do to utilize their insurance to the best of their ability is a good first step. Writing reports and analyzing the biggest managed care programs your office works for is the beginning of the process. Medical Billing Services can help with running and analyzing these reports.
Nowadays these companies are capable of working with several popular EMRs, such as eClincalWorks™, NextGen™, ADP Advancedmd™, Greenway™, Care 360™, Allscripts™, AmazingCharts™, Epic™, and several more. Once you know who the payers are, putting together patient literature can easily be accomplished with your insurance representative from that plan. They may even have information ready to go in flyers for you.
At MedicalBillingStar We can go a step further and assist with the training of your personnel and write scripts that are effective, professional, and consistent across the board with each employee in the office. We are here to help!!! Collecting money legally due to you is why we are here! Give us a call to see where we can assist today. MedicalBillingStar can bridge that gap between the payers and doctors office collections team.