Work smart; automate and outsource business processes!
The much anticipated Black Book survey findings are out and they indicate a strong possibility of medical practices undergoing a completer makeover! For years together physicians handled two very different and almost contradictory aspects of their workflow. It was a tight-rope walk between patient care and managing the business side of their medical practice.
The business side of medicine has almost become a catchphrase in the healthcare industry. There was no clear definition or a strategic plan to manage it. What was once regarded as a niggling pain, that one had to live with, has snowballed into a serious issue that demands to be dealt with. And dealt with immediately!
Shifting landscape makes it vital for practices to buckle up or die a quiet death!
There was a time, not very long ago, when physicians had to just take care of patients. The filing and transmitting of medical claims was something that the biller did. A cursory glance over the month’s collections was all that physicians did, as managing their medical practice’s finances was not their job.
The Affordable Care Act, which opened the doors to millions of uninsured, PQRS and Meaningful Use measures, an entirely new coding system and increased financial pressures, have shaken physicians out of their comfort zone. The alarming rate at which small medical practices shut their doors and the growing threat to the survival of independent practices, are a huge wake-up call across the entire healthcare continuum.
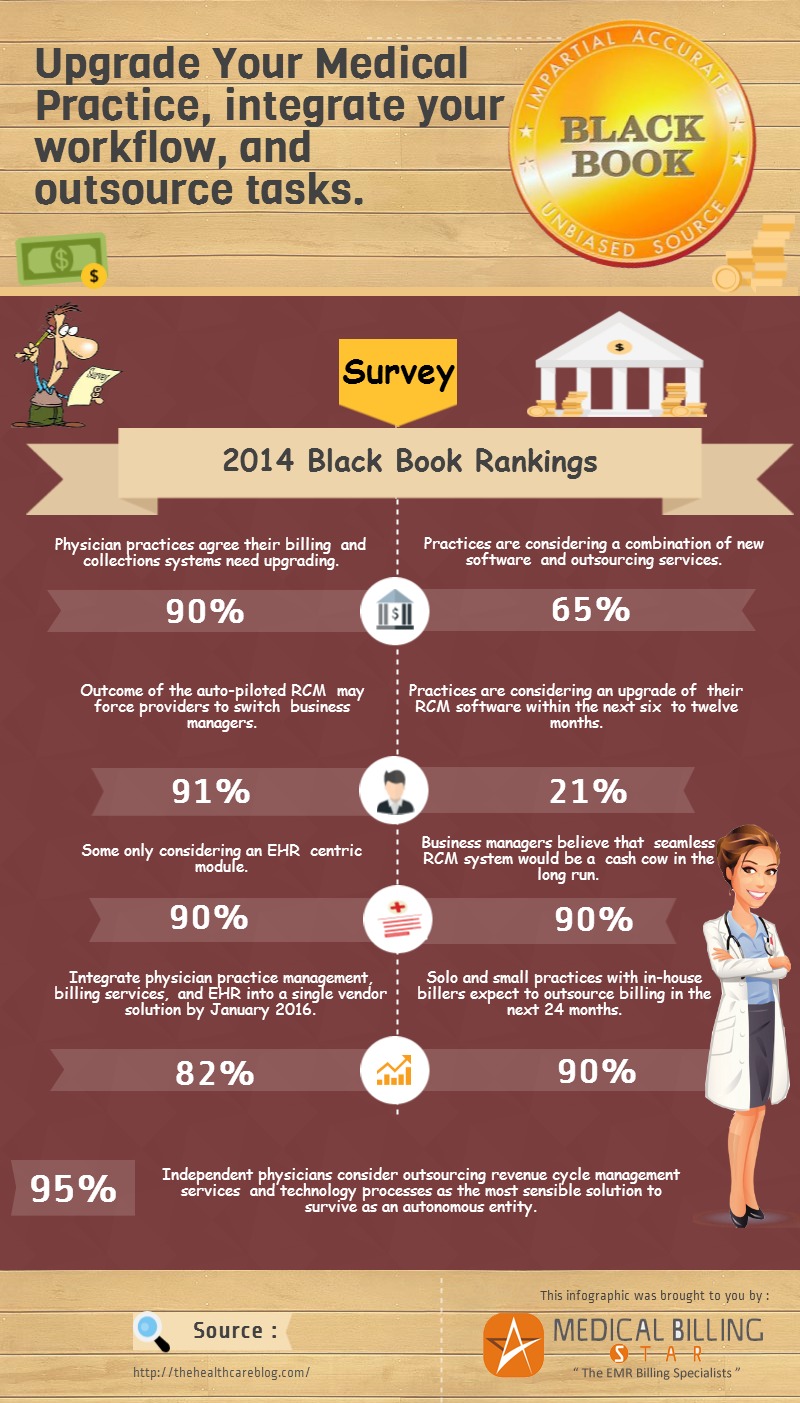
Desperate times call for desperate measures. The Black Book study that includes the perspectives and opinions of 400,000 respondents has indicated three emerging trends that are going to challenger the traditional way medical practices are going to function.
Upgrade, integrate, outsource…
This seems to be the magic formula that can save medical practices from drowning under a sea of reforms. Though most medical practices have finally got the hang of technology and are experimenting with different workflow models, there hadn’t be a clear sense of direction or collective change insofar.
Challenging old notions…
The Black Book survey challenges the common belief that physicians are still unwilling to let go of archaic methods of working.
There is a huge move to eliminate outdated software and about 21% of medical practices surveyed, are planning to upgrade their RCM software within the next 6 to 24 months.
91% of medical practice business managers feel that EHR systems that are not integrated with a full- fledged revenue management system can back their practices, further into a corner.
Facing the bitter truth!
The study also clearly illustrates that physicians are no longer in denial mode. About 90% of physicians surveyed admitted that their billing systems needed a facelift. There is also a huge demand for integrated systems so physicians will have to coordinate with a single point of contact. Speeding up workflow is the major objective of most medical practices and automating their workflow seems to be the perfect solution.
Utilizing system intelligence to perform business functions such as appointment scheduling, insurance eligibility checks, sending patient reminders and payment posting can quicken tasks and reduce headcount. Most medical practices still hire FTEs to perform tasks that their systems can do. Automating tasks can not only shorten the time taken to perform tasks but can also help in resource optimization.
Automating administrative functions: the way forward…
The administrative functions of medical practices can drive up efficiency. Prior to automating a process draw up a checklist of objectives and see whether through automating you actually end up saving time. Automating for the sake of automating can do more harm than good. Like investing in an automated voice recognition system and wasting productive time editing and correcting the transcripts.
Have a clear work-plan, educate staff about the software and strategy you are going to use and compare your existing process to the revised one, to make sure your switch to automation is successful. A spread-sheet that details the transition can ensure everybody in the medical practice is on the same page.
Creating a flow-map can standardize your automated processes and improve efficiency. You don’t want your staff to be bewildered by the sudden change in workflow processes. Listing out repetitive tasks is the easiest way of freezing on tasks that can be automated.
Here is what to automate…
Automating can be healthy but it can quickly turn into a major headache if not handled with caution. Medical practices should take care not to let their workflow processes spiral out of control. Though automation of tasks is common in other industries, automating workflow in the healthcare field is still at a nascent stage.
Here is a list of tasks that can be automated efficiently…
- A patient portal can automate everyday tasks to a large extent. Implement a patient portal that enables patients to fix up appointments based on available time-slots. Prescription refill requests can also be sent online. Patients can also be encouraged to pay online through a secure payment gateway.
- Setting up error prevention alerts and a thorough claim scrubbing tool or software can eliminate denials.
- Charge review alerts can reduce no-charges.
- E-prescribing allows physicians to communicate directly with pharmacies and can save medical practices from the tripwire of misplaced prescriptions.
- Setting up an email reminder or automated call reminders can reduce no-shows and late appointments.
- The ability to gather the financial performance data of a medical practice and track metrics will result in actionable and current financial being just a click away! This will help set targets and benchmarks.
There is no magic wand that can wipe away manual efforts completely!
Great! So now all physicians can just shop for software, or tool that can automate practice functions and go back to taking care of patients. But it is not as simple as that. The heterogeneity of workflow processes in a medical practice demand different methods of working. Automating completely, a practices business functions can prove to be counterproductive. As many as 90% of small medical practices and 95% of independent physicians are planning to outsource their medical billing and revenue cycle management functions and that could be because relying on tools alone cannot deliver the goods.
An increasing number of medical practices are downsizing to cope with financial bottlenecks and processes that were previously handled in-house are being outsourced. The increased need for outside expertise has been the major driver behind the shift to outsource business functions.
The bottomline…
It is the survival of the fittest out there! Healthcare organizations that successfully, integrate, automate, and outsource processes, will come out at the other end, more streamlined, productive and compliant.