Decide Here – Whether to Dwell-in or Leave the Page!
This article is especially designed to meet the needs of the physician practices and other healthcare delivery organizations that are looking for the tactics to revamp their medical billing process so as to boost your cash inflow.
Where the healthcare billing is travelling?
Though, physicians aren’t tethered to the aged technology and strategy, circumambient healthcare milieu may revoke your cerebral cortex due to diversified growth in healthcare information technology (HIT).
Do you have numerous “wh-questions” on your mind – pertinent to the funds management in your revenue cycle management (RCM) process? Then, this is the go-to technique to enliven your cash coffer.
MEDICAL BILLING STRATEGIES – 2014
Hoard your revenue in each phase of RCM!
Physician Credentialing and Contract Negotiation:
The federal payers have already fixed your reimbursement rates for the patient care services. Despite this, there is a dire need for the providers to negotiate with the payers to get lucrative reimbursements for the service rendered by you. Besides, abiding the payers’ rules during credentialing process brings you more savings.
Front-desk Collection:
Start collecting payments from the scratch – don’t let your staffs ignore the front-end tasks:
1. Point-of-service (POS) payments (Co-pays, deductibles, etc.).
2. Collection of dues well before patient encounter.
3. Thwarting denials through accurate eligibility verification.
4. Gathering insurance accurate data to avoid reimbursement disappointments.
Charge Capture:
HITECH Act, ACA’s “performance based payment” and other federal mandate are the driving forces that accentuate the ideal EHR implementation.
Charge capture must be done accurately for each encounter, procedure and surgery. Evolving ICD-10 guidelines call for the renovation of your super bills in sync with your clinical practice so that charge capture will be immaculate.
Claim Scrubbing:
This is the vital phase in the medical billing process that aid abridged AR process. AAPC/AHIMA certified coders must be a part and parcel of the claim scrubbing process – so that revenue loss due to underpayment and overpayment issues could be avoided. Concentrating on this phase greatly mitigates the claim rework cost.
Electronic Transmission:
Timed Clearinghouse transmission for fresh claims is one of the overlooked approaches in most practices. Large practices may need to file the scrubbed, “clean” claims daily.
Delay in addressing the rejected/denied claims with the remedial action may also hamper your cash in-flow.
eRemittance:
Interpretation of the remark codes and timely payment posting after the receipt of EOBs/ERAs is very essential for a successful RCM process. Besides, prompt cash inflow/ AR feed into the practice management system (PMS) or electronic medical/ health records (EMR/EHR) is mandatory to avert payment miss-outs and pointless follow-ups.
Denial Follow-up:
The denials must be addressed with an immediate effect to avoid delayed payments or re-denials. While working out on denials, the obligatory documents must be attached during re-submission or appeal. Though the cost involved in denial appeals or re-submissions is an additional burden, ignorance of denial management would be a serious pecuniary loss.
Patient Billing:
Don’t load your dice against yourself! Precision in the patient billing is a crucial point in the bill settlement. Inaccurate and difficult-to-read billing statements ensue in patient discontent, consequently culminating in bulldozed physician – patient relationship. Above all, a clear statement supports timely payment.
Resource Utilization:
Exploiting the resources like human resources, infrastructure, funds, technology, etc. to run a practice profitably is a master skill. Among that, leveraging the technology to satisfy patients and enhance practice profits is the challenging task. The following technology platforms ameliorate your patient experience, accelerate revenue cycle process and thus perk-up your business.
Practice Website:
- Patient portal
- Online forms and statements
- Online EHR access
- Online lab and imaging reports
- e-Payment support
- mHealth support (iPad, iPhone, Tablet, etc.)
- Chat support
- Healthcare News
- FAQs
- Social media (e.g. Facebook, twitter, etc.)
- Patient Blogs & forums
Benchmarking:
Setting a yardstick and working towards its accomplishment must be the prime goal, if you are attempting to reach your vision and mission.
What functions of the billing process that must be set in the yardstick achievement program?
1. Follow-up and retrieval of underpayments.
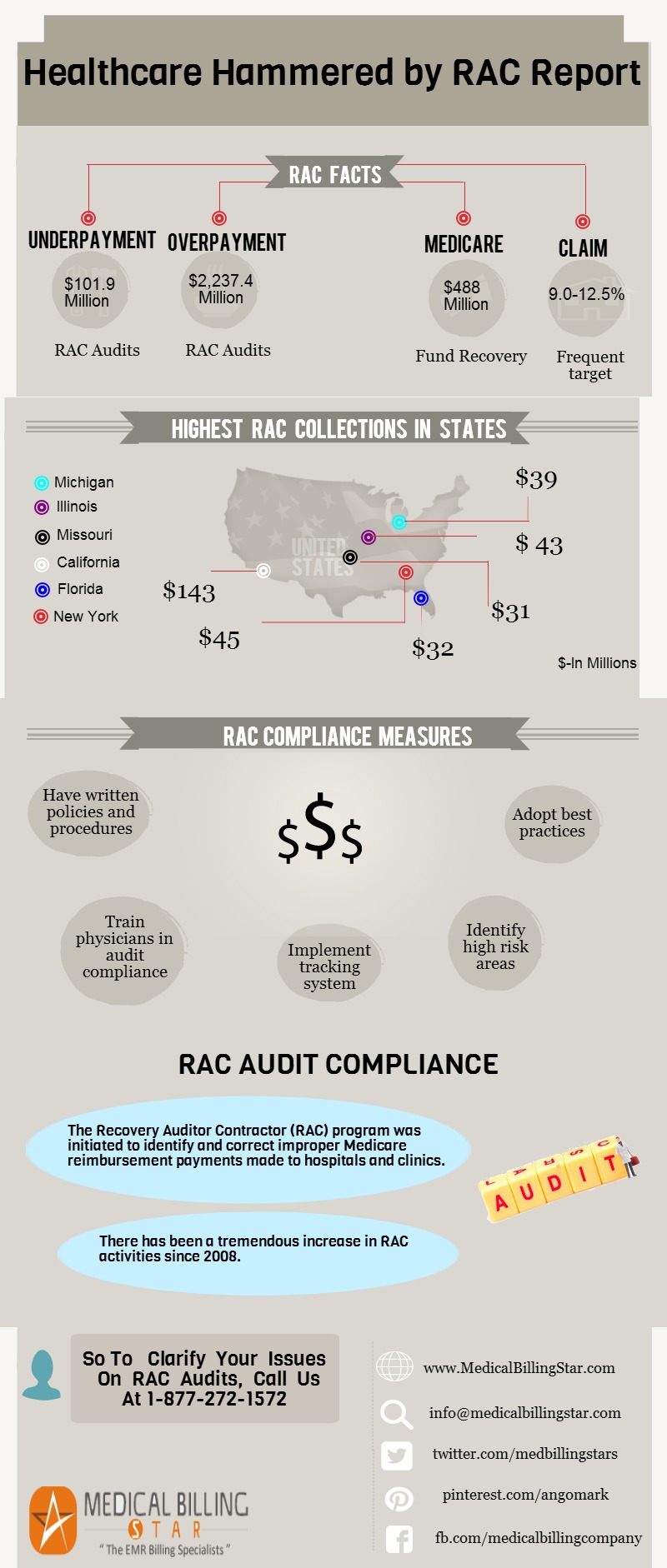
2. Averting penalties due to the breach of laws and audit policies (RACs, HIPAA, HITECH Act, etc.).
3. Aggressive follow-up of accounts receivables/bad-debts.
4. Evaluating and making small balance write-offs.
Besides, regular evaluation of your practice, process and finance must be done through the following reports:
- Practice Analysis Report
- RCM Analysis Report
- AR Summary Report
“PERSISTENT REVENUE INFLOW IS THE SINGLE PARAMOUNT WANT OF THE MEDICAL BILLING PROCESS”
Stretch your achievement from good to excellent with these proven medical billing strategies. It will be the hot topic in 2014 as most practices are going out-of-kilter due to stringent policies and other industrial factors.